How to Use Micro-Z™
Micro-Z Mini™ Operation Instructions
Silver-Thera™ Stocking Instructions
Silver-Thera™ Stocking Instructions
Features & Benefits
World's First Wearable DC Stimulator
The origins of DC stimulation date back 50+ years when it was invented for healing chronic wounds. The original devices were very large. So, we developed the world's first wearable DC stimulator along with the world's first glove and stocking electrodes. Now, with Micro-Z™ technology and Intelligent Textiles for Medicine™, you can prescribe stim therapy in your practice or have your patients take it home!
How Micro-Z™ Technology Works
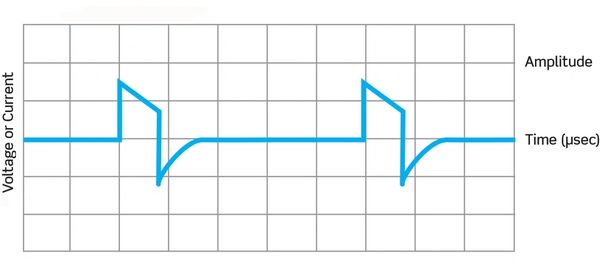
The Micro-Z™ is a direct current (DC) stimulator that delivers a monophasic twin peaked high voltage pulsed current (HVPC) in a micro-amperage range deep into the tissue bed to promote increase microcirculation, reduction of edema, which in turn promotes healing. Using the Micro-Z™ will help relieve pain and heal wounds while reducing muscle spasms and increasing range of motion.
Micro-Z™ Is Superior and Unique to TENS
Since the human body operates on DC signaling, the Micro-Z™ stimulates healing at the source of pain instead of masking it like traditional TENS electrotherapy. Micro-Z™ therapy effects the cells and vessels instead of stimulating the sensory nerves or causing muscle contractions.
No other device in the world delivers this unique electrical combination to promote healing.
- Direct Current - Parallels the body’s own electricity
- Shorter Pulses - Makes it more comfortable to the user
- High Volt - Greater force to push the energy deeper
- Low Amp Microcurrent - Effects cellular repair; Increases ATP production
Micro-Z™ Clinically Proven Benefits
- Increases microcirculation
- Promotes angiogenesis (the formation of new blood vessels)
- Reduces edema and inflammation
- Increases collagen production and alignment
- Decreases scar tissue formation
- Kills bacteria
- Increases fibroblast cells (needed for cellular repair)
- Increases white blood cell migration to site of injury
- Increases oxygen level in tissue
- Improves cell organization
- Increases ATP production
- Reduces pain due to healing of tissue
Micro-Z™ Clinically Proven Applications
- Acute/Chronic pain
- Muscle pain
- Joint pain
- Nerve pain
- Sports injuries
- Whiplash
- Wounds
- Fractures
- Sprains/Strains
Micro-Z™ vs. TENS
Micro-Z™ DC Stimulation
Micro-Z™ DC Stimulation
Micro-Z™ DC Stimulation

HVPC stimulation (direct current) creates an electrical field over the treated area that promotes increased microcirculation.
- Dosage in Microamps (millionth of an ampere).
- Deep tissue penetration through rapid ramp speed at 4 microseconds.
- Promotes micro blood circulation to relieve pain at the origin.
- Helps relieve muscle spasms.
- Reduces edema and inflammation.
- Promotes healing.
- Antibacterial.
- Daytime AND nocturnal treatment programs.
TENS AC Stimulation
Micro-Z™ DC Stimulation
Micro-Z™ DC Stimulation
Transcutaneous stimulation (alternating current) delivers a low-frequency (<50 Hz) alternating current to a focused treatment area. Due to the nature of low-frequency, however, these signals have a low capacity to overcome skin resistance – resulting in these units only providing temporary pain relief while being worn.
- Dosage in Milliamps (thousands of an ampere).
- Shallow tissue penetration through slow ramp speed at 40 microseconds.
- Blocks the pain signal from the brain acting as an antagonist to nerves.
Micro-Z™ Instructions for Use
- Make sure the skin is clean on the treatment area.
- Snap Micro-Z Mini™ or Micro-Z II™ lead wires into the back of the device.
Place the lead wires on the back of the Micro-Z Mini™ or Micro-Z II™, making sure that the Black button (-) is attached to the negative snap and that the red button is attached to the positive (+) snap. - Place the two (2) AAA in battery compartment.
- Place the Micro-Z Mini™ or Micro-Z II™ 3” round electrodes to the red and black lead wire pins. And then place the black lead wire /electrode furthest away from the heart on a muscle bed and the red lead wire four to five inches away on another muscle. (see photos illustrations below here)
- Turn on the Micro-Z Mini™ or Micro-Z II™ by pushing down the On/Active button on the left hand side of the Micro-Z Mini™ or Micro-Z II™; this on switch actives the device for a 30 minute treatment P1; by pushing the right hand button this activated the 8 hour treatment P2.
- P1 is a 30 min. treatment and if selected the Micro-Z Mini™ or Micro-Z II™ will automatically turn off after the 30 min. treatment is complete.
- P2 is an 8 hour treatment where the Micro-Z Mini™ or Micro-Z II™ will cycle on and off automatically over 8 hours. It will be on for 20 min and off for 40 min. during the treatment period.
- Then pump the increase button (+) to light sensation or comfort level and then you can reduce sensation by decrease button (-) to below sensory feeling. Note: that using the 8 hour treatment at night while sleeping the therapeutic level of stimulation is always below sensory
- The Micro-Z Mini™ or Micro-Z II™ will turn off automatically once the 30 min (P2) or 8 hr. (P2) treatments are completed. If you want to stop the stimulation, hold down the button On/Active for 5 seconds.
- If you experience any skin irritation, stop the therapy and consult your clinician.
- The Micro-Z Mini™ or Micro-Z II™ is very safe to use and you should use them as often as you can both daily as well as at night.
Micro-Z™ Troubleshooting Guide
- Are the batteries dead? – Micro-Z™ runs on 2 AA batteries.
Solution: Replace the batteries - Are the batteries properly oriented in the battery compartment?
Solution: Make sure the that (+) pole is connected to the (+) end. Same for (-) pole. - Have the electrodes dried out?
When you place the electrodes on your skin they should feel slightly wet, and when you pull them off they should still feel sticky. If neither of these is the case, then replace them. The whole electrode should have contact with the skin, and there should be no curled edges.
- Are the batteries dead? – Micro-Z™ runs on 2 AA batteries.
Solution: Replace the batteries. - Have the leads fallen off?
Solution: Are the electrodes moving under your clothes so that contact with the skin is lost? Experiment with the way that the leads hang when they are in place. Try securing the electrodes with micropore tape around the edges. - Are the electrodes past their effectiveness?
Solution: If the electrodes feel dry or have lost their stickiness, replace them with a fresh pair. - Have you become tolerant to the signal strength?
Solution: As you become more confident with using your Micro-Z™, you may find that you will benefit from higher signal strengths. Try increasing the (+) power output to see whether this is the case.
- Try varying the position of the electrodes, and the length of time of contact with the skin.
- Sometimes pre-treating the skin with low strength hydrocortisone cream can reduce the severity of a reaction. If symptoms persist, please speak to your doctor.
- Try using different manufacturers electrodes (which may have different chemicals in the adhesive).
Micro-Z™ Wound Healing Suggested Protocols
Electrical stimulation is defined as the use of an electrical current to transfer energy to a wound. The type of electricity that is transferred is controlled by the electrical source. Capacitatively coupled electrical stimulation involves the transfer of electric current through an applied surface electrode pad (capacitatively coupled) with the external skin surface and /or wound bed. When capacitatively coupled electrical stimulation is used, two electrodes are required to complete the electric circuit. Electrodes are usually placed 2’ to 3’ bracketing the wound on skin.
When discussing electrical stimulation, it is important to distinguish the waveform used for the protocol. Although there are many waveforms available on electrotherapy equipment, the one that has the most thorough and consistent evaluation in vitro, in animal studies and in controlled clinical trials is monophasic twin peaked high voltage pulsed current ( HVPC). The pulse width varies with a range from 20-200 microseconds. The HVPC devices also allow for selection of polarity and variation in pulse rates both of which seem to be important in wound healing. It is a very safe current because it’s very short pulse duration prevents significant changes in both tissue pH and temperature. Therefore, the most tested and safe type of stimulation is the one recommended.
Other types of waveforms and have been tested in clinical trials but will not be discussed here due to limited space.
Overview
Acceptance of electrical stimulation for wound healing by the medical community has been a long and complex task. In 1994, the Agency for Health Care Policy and Research (AHCPR) panel issued Treatment of Pressure Ulcers, Clinical Practice Guideline, Number 15. The panel of pressure ulcer care experts used an explicit science-based methodology and expert clinical judgment to develop statements regarding pressure ulcer treatment. Extensive literature searches, critical review and synthesis were used followed by peer and field review to evaluate the validity, reliability and utility of the guideline in clinical practice. AHCPR panel issued a statement about use of electrical stimulation as an adjunctive therapy for pressure ulcers: ” Consider a course of treatment with electrotherapy for Stage III and IV pressure ulcers that have proved unresponsive to conventional therapy. Electrical stimulation may also be useful for recalcitrant Stage II ulcers. Strength of Evidence = B.” The panel found that data from 5 clinical trials involving 147 patients to support the effectiveness of this therapy for pressure ulcers.
Bioelectric System
The body has its own bioelectric system. This system influences wound healing by attracting the cells of repair, changing cell membrane permeability, enhancing cellular secretion through cell membranes and orientating cell structures. A current termed the “current of injury” is generated between the skin and inner tissues when there is a break in the skin. The current will continue until the skin defect is repaired. Healing of the injured tissue is arrested or will be incomplete if these currents no longer flow while the wound is open. A moist wound environment is required for the bioelectric system to function. A rationale for applying electrical stimulation is that it mimics the natural current of injury and will jump start or accelerate the wound healing process.
Research Wisdom
Keeping a wound moist with normal ( 0.9% ) saline ( sodium chloride ) maintains the optimal bioelectric charge because it is like the electrolytic concentration of wound fluid. Dressings such as amorphous hydrogels and occlusive dressings help promote the body’s “current of injury” by keeping the wound moist.
Debridement and Thrombosis
Debridement is helped if the tissue is solubilized such as with enzymatic debriding agents. ES using negative current has been shown to solubilize clotted blood. Necrotic tissue is made up of coalesced blood elements. The negative pole has been used to begin treatment in all controlled clinical studies and most of the wounds have necrotic tissue. This research would lend support to that part of protocol. The positive electrode has been found to induce clumping of leukocytes and forming of thrombosis in the small vassals this was reversed with the negative electrode. (Gentzkow 91) This may explain a clinical observation that hematoma or hemorrhaging at the wound margin or on granulation tissue are dissolved and reabsorbed following application of HVPC with the negative pole. Hemorrhagic material goes on to necrosis if not dissolved and reabsorbed quickly.
Clinical Wisdom
Clinical experience has repeatedly shown that treatment with the inflammation protocol, using negative polarity, promotes rapid absorption of hemorrhagic material, usually within 48 hours.
Clinical Wound Healing Studies
Early studies using direct current stimulation reported long treatment times of 20-40 hours per weeks. Four controlled clinical studies and three uncontrolled studies with HVPC report a mean healing time of 9.5 weeks with 45-60 minute treatment 5-7x/wk.
Summary of Scientific Rationale for Application
Electrical stimulation affects the biological phases of wound healing in the following ways:
- Initiates the wound repair process by its effect on the current of injury
- Increases blood flow
- Promotes phagocytosis
- Enhances tissue oxygenation
- Reduces edema perhaps from reduced microvascular leakage
- Attracts and stimulates fibroblasts and epithelial cells
- Stimulates DNA synthesis
- Controls infection ( Note: HVPC proven bacteriocidal at higher intensities than use in clinic and may not be tolerated by patient)
- Solubilizes blood products including necrotic tissue
Proliferation Phase
- Stimulates fibroblasts and epithelial cells
- Stimulates DNA and protein synthesis
- Increases ATP generation
- Improves membrane transport
- Produces better collagen matrix organization,
- Stimulates wound contraction
Epithelialization Phase
- Stimulates epidermal cell reproduction and migration
- Produces a smoother, thinner scar
Use and application of the modality is not pathology dependent.
Types of wounds for which there is indication to use HVPC include:
- Pressure Ulcers Stage I through IV
- Diabetic ulcers due to pressure, insensitivity and dysvascularity
- Venous Ulcers
- Traumatic Wounds
- Surgical Wounds
- Ischemic Ulcers
- Vasculitic Ulcers
- Donor Sites
- Wound Flaps
- Burn wounds
The protocols change as the wound healing phase changes. Assessment and diagnosis of the wound healing phase determines the treatment protocol.
Protocol for treatment:
- Necrosis free
- Erythema free
- Edema free
- Exudate free
- Red granulation
Stimulator Settings:
- Polarity – Place the negative pole distal and positive pole proximal to the wound on a muscle mass.
- Pulse rate – 100 for 15 min and 10 PPS for 10 min
- Intensity – 50 volts
- Duration – 60 minutes or two P1
- Frequency 5-7 x per week, once daily
Research Wisdom: Use of Amorphous Hydrogel for Conduction
A saline based amorphous hydrogel, which has the ability to conduct electric current has been tested and the conductivity is comparable to saline. Whether the healing of the wound is improved when this product is used for conducting current and then left in the wound has not been tested. In the meantime, such a product may have the added advantage of being used as the wound dressing to keep the wound moist after the electrical stimulation treatment is completed.
Setting Up the Patient
- Have supplies ready before undressing the wound.
- Position patient for ease of access by staff and comfort of both.
- Remove the dressing and place in an infectious waste bag.
- Cleanse wound thoroughly to remove slough, exudate and any petrolatum products
- Sharp debride necrotic tissue, if required, before HVPC treatment
- Open gauze pads and fluff, then soak in normal saline solution, squeeze out excess liquid. An alternative is to use an amorphous hydrogel impregnated gauze. Hydrogel sheets can also be used to conduct current under the electrodes
- Fill the wound cavity with gauze including any undermined/tunneled spaces. Pack gently.
- Place a negative electrode 2” to 3” distal to the wound on a muscle mass.
- Connect to stimulator lead
- Positive electrode placement:
Usually placed proximal electrode 2” to 3” from the wound. Place over soft tissues a muscle mass, avoid bony prominences.
Clinical Wisdom: Remove Petrolatum Before Stimulation
All petrolatum products including enzymatic debriding agents such as collagenase, Santyl, fibrinolysin, and Elase, which are petrolatum-based products, must be removed before treatment or current will not be conducted into the wound tissues.
Aftercare
After the electrical stimulation treatment is complete, slip the electrode out. The wound can be left undisturbed. If additional topical treatments are required such as enzymatic debriding agents or antibiotics, then the packing will need to be removed, topical agent applied and redressed.
Research Wisdom: Avoid Wound Chilling
Frequent dressing changes are being discouraged because it disturbs the wound healing environment by removing important substances in wound exudate and cooling the wound. It takes three hours for a chilled wound to re-warm and slows leukocytic and mitotic activity
Signs of adverse effects were evaluated in the various clinical trials and none were found except some skin irritation or tingling under the electrodes in a few cases. Patients with severe peripheral vascular occlusive disease (PVD), may experience some increased pain, usually described as throbbing, in the leg after electrical stimulation.
Contraindications for treatment with electrical stimulation include the following:
- Placement of electrodes tangential to the heart
- Presence of a cardiac pacemaker
- Placement of electrodes along regions of the phrenic nerve
- Presence of malignancy
- Placement of electrodes over the carotid sinus
- Placement of electrodes over the laryngeal musculature
- Placement of electrodes over topical substances containing metal ions
- E.I. povidone iodine and mercurochrome, unless thoroughly cleaned.
- Placement of electrodes over osteomyelitis
Prizm Medical Inc.
940 Sherwin Parkway, Buford, Georgia 30518, United States